Tarsal Tunnel Syndrome
What is Tarsal Tunnel Syndrome?
Tarsal tunnel syndrome refers to symptomatic compression of the posterior tibial nerve branches within the tarsal tunnel.
It is an uncommon cause of heel pain.
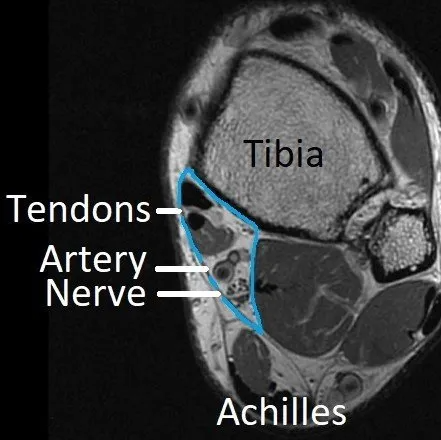
The tarsal tunnel is a passage from the leg to the foot behind the inner (medial) ankle (see image and Achilles & Heel - Anatomy and Imaging). Tendons, blood vessels and nerves pass through it (area outlined in blue).
The tarsal tunnel cannot expand so swelling inside it presses on the nerves and causes pain and sensory changes under the foot. This is similar to carpal tunnel syndrome in the hand.
Causes of Tarsal Tunnel Syndrome
Any mass or swelling inside the tarsal tunnel can cause tarsal tunnel syndrome. Common reasons are ganglions, bone spurs and varicose veins.
Associated or mimicking conditions:
- Severe flat foot deformity can stretch the nerves supplying the bottom of the foot.
- Diabetes mellitus and other medical conditions can cause nerve dysfunction (peripheral neuropathy).
- Spinal nerve compression and "sciatica".
Symptoms of Tarsal Tunnel Syndrome
Most individuals with tarsal tunnel syndrome complain of pain, numbness and burning or tingling sensations on the bottom of the foot and heel (see image).
Diagnosis of Tarsal Tunnel Syndrome
Tarsal tunnel syndrome may take time to diagnose as not all health practitioners have seen it before. The mimicking conditions mentioned above are often thought of first as they are more common.
The diagnosis requires:
- history taking
- examination, including a Tinel's sign (tapping the posterior tibial nerve reproduces symptoms)
- investigations.
Investigations to confirm the diagnosis and determine the cause include ultrasound, CT, MRI and/or nerve conduction studies.
Treatment of Tarsal Tunnel Syndrome
Tarsal tunnel syndrome can be treated non-surgically by:
- anti-inflammatory medications
- cortisone injections into the tarsal tunnel
- orthotics to support the arch of the foot and take tension off the tibial nerve.
Surgery is only offered when the diagnosis is confirmed and a mass (ganglion, bone spur, varicose vein, etc) is present within the tarsal tunnel.
When symptoms are severe or sole of foot numbness is developing, urgent tarsal tunnel release is required. Otherwise, non-surgical treatment is tried for several months.
Surgery involves releasing the tarsal tunnel and tight muscle bands over the tibial nerve branches. Any masses are carefully removed and the nerve branches examined.
This procedure requires a bandage and crutches for 2 weeks then three months until most healing has occurred. 90% of people are improved by surgery if it is done for the right reasons.
Please see General Information about Surgery in the TREATMENTS menu.
Dr Beamond performs this surgical procedure. However, when imaging shows severe scarring around the nerves, he recommends a plastic surgeon or neurosurgeon with micro-surgical skills do it for safety reasons.