Rupture of the Achilles tendon is most commonly seen in middle-aged men trying to remain active. Women are less likely to have this injury.
People with Achilles tendinopathy, obesity, diabetes, gout, inflammatory arthritis and on certain medications (steroids, ciprofloxacin antibiotics) are at higher risk of Achilles tendon rupture. What causes an Achilles Tendon Rupture?
Achilles tendon ruptures mainly occur in people playing recreational sports that involve running, pivoting and jumping, but can happen to anyone, including elite athletes.
Sports associated with Achilles tendon rupture include:
- soccer
- football
- netball
- basketball.
All of these sports involve rapid push-off and change of direction (eccentric contraction).
Interesting facts: David Beckham tore his left Achilles tendon playing for AC Milan in 2010. He had it repaired in Finland. Symptoms of Achilles Tendon Rupture
When the Achilles tendon ruptures, people experience:
- severe pain in the Achilles and up the calf, making it difficult to walk
- swelling and bruising
- leg weakness and difficulty standing on tiptoe or using stairs.
A popping or snapping sound may be heard when the injury occurs.
Diagnosis of Achilles Tendon Rupture
The diagnosis of Achilles tendon rupture is usually straight-forward, and based on:
- symptoms
- physical examination.
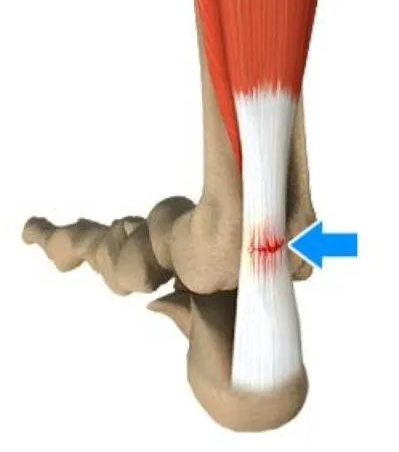
A gap in the tendon, four to six centimetres above heel bone, is usually present (see images below). Gently squeezing the calf muscle helps determines if there is a connection between the calf and heel bone. If the Achilles tendon is intact, there will be flexion movement of the foot. If it is ruptured, no movement occurs.
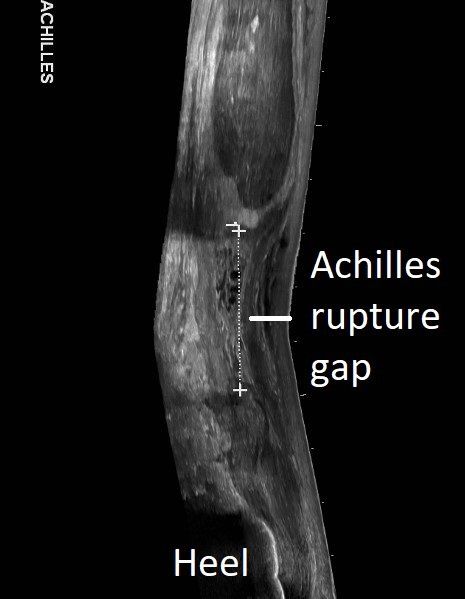
Unless the diagnosis is unclear or complicated by previous Achilles injury, no investigations are absolutely needed. Ultrasound shows the rupture and how much of a gap is present between the ends. MRI is usually only required in missed Achilles tendon rupture or if severe Achilles tendinopathy
is suspected.
Achilles rupture gap - ultrasound
Button
Treatment of Achilles Tendon Rupture
Achilles tendon rupture can be treated by
non-surgical or surgical methods. There have been many studies on this over the last 15 years. At one year after rupture, both types of treatment can have good outcome.
Both non-surgical and surgical treatments have become more advanced. Surgery allows earlier return to full activity out of a boot but has the small risks of anaesthesia and a surgical incision. Re-rupture rate is higher in non-surgically treated people.
For these reasons, both treatment options are discussed. In general, young active people do well with surgery and those with medical conditions are treated without surgery. Physiotherapy is recommended in all cases.
Non-surgical treatment of Achilles tendon rupture
Non-surgical treatment involves wearing a "moon-boot" 24 hours/day, initially with three wedges under the heel. This brings the tendon ends together, allowing healing. The wedges come out over six weeks and the boot comes off after ten weeks.
It is very important that the toes remain pointing down
at all times during the first three weeks after rupture. This must be remembered when putting on socks and washing.
Conversion to surgical treatment can occur if healing is not occurring.
Surgical treatment of Achilles tendon rupture
Achilles tendon repair surgery brings the ends of the tendon together with sutures. This is done using small incisions in most people.
A "moon-boot" is worn full time for six weeks then only to walk for two more weeks. Wedges under the heel come out over the first six weeks.
Untreated Achilles Tendon Rupture
If an Achilles tendon rupture is allowed to go untreated, most people will have significant leg weakness and wasting. Plastic splints or complex reconstructive surgery is required.